Abstract
Background: Several reports have been published assessing anti-SARS-CoV-2 antibody reactions and T-cell responses against SARS-CoV-2 using spike protein peptide-stimulated interferon-gamma release assays after vaccination among patients with plasma cell dyscrasias or lymphoma. However, no reports have investigated entire T-cell clones against SARS-CoV-2 using deep next-generation sequencing (NGS) to clarify the whole T-cell reaction against each vaccine-targeted peptide.
Methods: We retrospectively assessed antibody and T-cell responses in 74 patients with multiple myeloma (MM), two with malignant lymphoma (ML), and 21 healthy individuals (HIs) who received two-dose mRNA vaccination (BNT162b2), 21 days apart. Serum and peripheral blood samples were collected on day 1 (T0; before the first dose) and on days 27-142 (T2; 1-17 weeks after the second dose), if available. Antibody responses were analyzed using Elecsys® Anti-SARS-CoV-2 (Roche). This system allows for the quantitative detection of antibodies, predominantly IgG, and may also capture IgM and IgA, targeting the SARS-CoV-2 spike (S) protein receptor-binding domain (RBD) and nucleocapsid (N) protein. As suggested by the manufacturer, cut-off index (COI) values of S-IgG ≥ 0.8 U/mL and N-IgG ≥ 1.0 were considered positive. T-cell responses were assessed by immunosequencing the CDR3 regions of TCRβ using the deep-immunoSEQ® Assay (Adaptive Biotechnologies, Seattle, WA, USA), as previously described (Alter G et.al., Nature 2021). Clonal depth was defined as the sum frequency of COVID-19 specific TCRs in the repertoire, which was calculated as the total number of COVID-19 specific T cells divided by the total number of T cells in the sample.
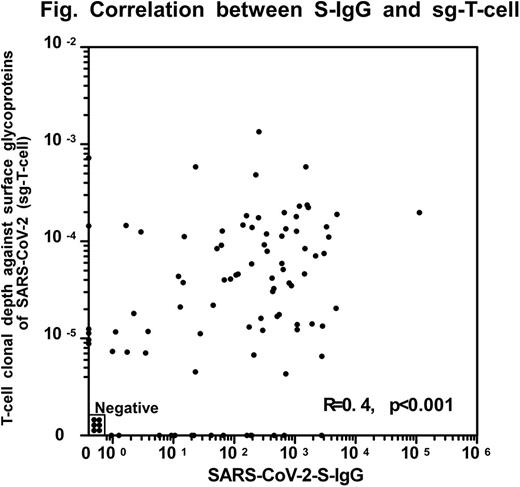
Results: A total of 74 patients with MM (30 males, 44 females; median age, 73 years), two male patients with ML (median age, 77.5), and 21 HIs (8 males, 13 females; median age, 64 years) participated in this study. Two patients with ML were included because they showed SARS-CoV-2 PCR positivity for more than two months, despite appropriate treatment. Based on CoV-N values, none of the participants except for one patient whose data was not available experienced a COVID-19 infection before vaccination. Anti-CD38 monoclonal antibody (mAb) was administered within 6 months before the first anti-SARS-CoV-2 vaccination to 24 of 74 (32%) patients with MM. The relationship between S-IgG and T-cell clonal depth against the surface glycoproteins of SARS-CoV-2 (sg-T-cell) showed a moderate correlation (Figure: r=0.4, p<0.001). S-IgG-negativity was observed in 12 of 76 patients with MM or ML (16%), but none of the HIs, while sg-T-cell undetectable was in 20 of 76 patients with MM or ML (26%) and was in only one of 21 HIs (5%). Among the 12 patients with negative S-IgG after vaccination, six achieved sg-T-cell levels higher than 8 x 10-6 (50%). Regarding COVID-19 specific immune responses between patients with MM and HIs, sg-T-cell levels in patients with MM were lower than those in HIs (p=0.046). Additionally, S-IgG levels in patients with MM were also lower than those in HIs (p<0.001). Furthermore, S-IgG levels in patients with MM who received anti-CD38 mAbs within six months prior to their first anti-SARS-CoV-2 vaccination were lower (p=0.01), as were their sg-T-cell levels (p=0.02), than those without anti-CD38 mAbs. This finding suggests that humoral response and T-cell immunity were impaired in patients with MM who received anti-CD38 mAbs. After vaccination, seven patients (five with MM and two with ML) experienced breakthrough COVID-19 infections. Among them, three were S-IgG-negative, three were sg-T-cell undetectable, and one was S-IgG-negative and sg-T-cell undetectable. Two patients died of COVID-19, and the other two died of MM and ML, respectively.
Conclusions: According to the results of this study of humoral and cellular immune responses after vaccination against SARS-CoV-2, the T-cell response is not closely related to the IgG response. Furthermore, IgG and T cells specific to SARS-CoV-2 spike proteins might be essential for preventing COVID-19 infection and severity. This finding suggests the importance of T-cell immunity surveillance. To confirm the generalizability of our findings, large-scale studies are needed in the future.
Disclosures
Takamatsu:Bristol-Myers Squibb: Honoraria; Sanofi: Honoraria; Ono: Honoraria; Janssen: Honoraria; SRL: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal